Dr. Sikha Mukhopadhyay,
Ex-Associate Professor of Psychiatry,
I.P.G.M.E.R., Kolkata
 Mental illnesses are disorders of thoughts, emotions, and behaviour. These constitute a large part of the global burden of diseases.
Mental illnesses are disorders of thoughts, emotions, and behaviour. These constitute a large part of the global burden of diseases.
Yet they do not get sufficient importance or the attention they deserve by our society and by our governments. This to a large extent due to the still prevalent stigma associated with the diagnoses of mental illness. Poor knowledge of mental health is a key factor that contributes to inadequate mental health services.
This often leads to a large gap between the needy and who ultimately receive psychiatric treatment.
To understand the severity of the burden of mental illnesses it is advisable to consider some mental health related statistics from the world over and from India in particular. In 1990, five of the top ten leading causes of disability worldwide were from mental illnesses, accounting for almost a quarter of the total years lived with disability (Murray and Lopez 1996).
More recent estimates indicate that disability from mental illness and substance abuse disorders has grown from 5.4% of all disability adjusted years of life worldwide in 1990, to 7.4% of the same in 2010 (Whiteford, Degenhardt et al. 2014). Community based epidemiologic surveys show the life-time prevalence of mental disorders to be as high as 50% and the one-year prevalence to be as high as 30% depending on the country (Kohn, Saxena et al. 2004).
In India, a study by the Indian Council of Medical Research in 2017 estimated that about one in every seven persons suffer from mental disorders of varying severity, with depression and anxiety disorders being the most common mental disorders, affecting 45.7 million and 44.9 million people respectively (Sagar, Dandona et al. 2020). The same study also reported a significant increase in the incidence of mental health disorders in India over the years, with reported increases in cases of depression, anxiety disorders, schizophrenia, bipolar disorders, intellectual disability, conduct disorders and autism.
Mental illness is an umbrella term that encompasses different disorders each with its own pathology, with the common thread among all being manifesting changes in the behaviour of the affected individual. As a result, a wide range of variability is seen in the duration of mental illnesses and in their qualitative presentations in the clinic.
Some disorders are acute-onset with presentations of sudden and severe behavioural abnormalities, whereas other disorders manifest over longer duration of time and are associated with progressive behavioural changes. The latter types are often referred to as chronic disorders because they unfold over longer stretches of time.
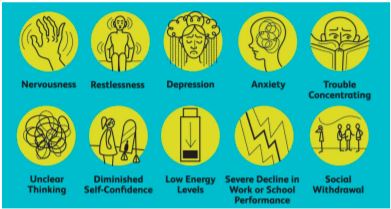
Symptoms of mental illnesses are also varied– some patients remain withdrawn and aloof when first brought in, whereas others may be violent and aggressive posing a threat to themselves and to others.
It is this behavioural unpredictability of the mentally ill that unfortunately leads the public to see them as being more dangerous than warranted and to treat them as social outcasts.
Since the domain of psychiatric illnesses is vast, I have tried to provide a simplified non-technical description of the types of mental disorders commonly encountered in clinical practice with the hope that this may educate and further create awareness on mental health in the community.
 Psychiatric illnesses are broadly divided into psychotic disorders, in which reality testing (the ability to perceive objects or events as they are) is lost, and neurotic disorders in which reality testing is preserved. Both psychotic and neurotic disorders may be of varying degrees of severity. In the following paragraphs, I briefly discuss some major psychiatric illnesses and conditions commonly encountered.
Psychiatric illnesses are broadly divided into psychotic disorders, in which reality testing (the ability to perceive objects or events as they are) is lost, and neurotic disorders in which reality testing is preserved. Both psychotic and neurotic disorders may be of varying degrees of severity. In the following paragraphs, I briefly discuss some major psychiatric illnesses and conditions commonly encountered.
Schizophrenia
A major psychotic disorder is schizophrenia. Schizophrenia literally translates as ‘split mind’. In this disorder there is a loosened association between thought, emotion, and behaviour.
The absence of reality tests leads to hallucinations (false perceptions without stimuli, for instance seeing someone when there is nobody), delusions (firm belief in an idea despite evidence to the contrary) and consequent odd behaviour.
 Other common behavioural changes associated with schizophrenia include neglect of personal care and hygiene, impaired social and occupational functioning and disturbances of sleep and appetite.
Other common behavioural changes associated with schizophrenia include neglect of personal care and hygiene, impaired social and occupational functioning and disturbances of sleep and appetite.
Usually, schizophrenia starts early in life between 15 to 35 years of age. At its initial onset patients experience hallucinations and delusions and over time they may become socially withdrawn, quiet and apathetic if left untreated.
Schizophrenia affects about 1% of the population, both male and female, in equal proportion. Schizophrenia can be managed by using a combination of medications and psychotherapy.
 Patients’ families also need to be educated about the illness and its symptoms to help them better understand the affliction and the problems that patients face.
Patients’ families also need to be educated about the illness and its symptoms to help them better understand the affliction and the problems that patients face.
With proper medical care many patients with schizophrenia can be rehabilitated; statistically, one third of treated patients can live a normal life, another third can function reasonably well despite persistence of symptoms.
The remaining one-third of patients however may remain markedly impaired and need frequent hospitalisation.
Overall, early medical intervention in patients diagnosed with schizophrenia is associated with better overall quality of life.
Bipolar Mood Disorder
In this disorder the patient’s mood fluctuates between extreme elevation (also termed the manic phase) and extreme depression. During manic phases patients become hyperactive and excessively talkative and show a reduced need for sleep.
 Their mood may be elevated or irritable. Some patients may also have grandiose ideas and increased risk-taking tendencies and may become angry and violent if contradicted or crossed.
Their mood may be elevated or irritable. Some patients may also have grandiose ideas and increased risk-taking tendencies and may become angry and violent if contradicted or crossed.
Symptoms of depression in bipolar patients resemble those of depression in general which is independently discussed.
Anxiety frequently accompanies other symptoms in patients with bipolar disorder in both their manic and the depressed phases.
Symptoms associated with anxiety are also independently discussed later. Bipolar mood disorder affects about 1% of the population. This disorder can also be managed using medications, psychotherapy, and electro-convulsive therapy.
Depression
In patients with depression mood is pervasively low for most of the day and most of the days of the week, for at least two weeks. Patients report loss of energy, losing interest in previously pleasurable activities, feelings of helplessness, hopelessness for the future and of feeling like a failure.
 Left untreated severe depression may lead to suicidal thought and ultimately the act of committing suicide.
Left untreated severe depression may lead to suicidal thought and ultimately the act of committing suicide.
False beliefs formed by severely depressed patients may even lead them to committing acts of homicide or infanticide. Major depressive disorder occurs in 2-3% of men and 5-10% of women. Symptoms of depression can be significantly relieved using appropriate medications and by psychotherapy.
Anxiety disorders
The defining symptoms associated with anxiety disorders are -mental apprehension of the anxiety triggering situation, physical tension, physical symptoms leading up to a state of heightened alertness (like palpitation, shaking, dry mouth) and dissociation (in psychiatry dissociation refers to a state where a person loses awareness of his own identity (that is dissociates from themselves) such as seen in multiple personality disorders. This sense of identity loss is often an adaptive response for coping with past traumas and temporarily reduces feelings of fear, shame, or anxiety in the sufferer). Some specific examples of disorders grouped under this term are -generalised anxiety disorder, phobic anxiety disorder and panic disorder.
Besides these, there are other disorders such as obsessive-compulsive disorder, post-traumatic stress disorders where symptoms of anxiety disorders predominate but are mixed in with other behavioural abnormalities.
Some special cases of anxiety disorders are described below.
Generalised anxiety disorder-Patients with this disorder experience long-lasting anxiety that is not focused on any one object or situation. There is a non-specific, persistent fear and worry and an excessive concern with everyday matters.
This happens to be the most common anxiety disorder affecting older adults.
Phobic anxiety disorder- Here anxiety is triggered by a specific stimulus or situation. Between 5% and 12% of world population suffer from phobic disorders such as arachnophobia- a fear of spiders, or ophidiophobia- a fear of snakes. Psychotherapy and behavioural therapy (such as ‘flooding’- where the patient is exposed to the anxiety triggering stimulus in a safe environment until their fear/anxiety abates) are common treatments.
Agoraphobia – This is a specific anxiety disorder about being in a place or situation where escape is difficult or embarrassing, or where help may be unavailable.
Social anxiety disorder – In this case patients suffer intense fear of negative public scrutiny, public embarrassment, humiliation, or social interaction. This fear can be specific to particular social situations (such as public speaking) or more typically, in almost all social interactions.
Obsessive-compulsive disorder (OCD) – This is a type of anxiety disorder where patients experience repetitive, distressing, persistent, and intrusive thoughts (obsessions) and irrepressible urges to perform specific acts or rituals in response to these thoughts (compulsions). It occurs in 3% of the population. It may become chronic and disabling if untreated.
Post-traumatic stress disorder (PTSD) – This is an anxiety disorder which results from a life threatening traumatic experience where the patient experiences disturbing flashback memories of the experience that in turn triggers severe anxiety.
In general anxiety disorders may be treated using medications, psychotherapy, and behavioural therapy (such as relaxation exercises, mindfulness meditation etc.). Physical exercise has also been shown to be very effective at alleviating anxiety. For phobic anxiety disorders, patients are advised to not avoid situations that induce anxiety but rather to develop healthy coping strategies to face their challenges, since avoidance further reinforces phobias.
Substance use disorders
Substance use disorders refer to the use of psychoactive substances like alcohol, cannabis, opium, tobacco, sleeping pills etc in a harmful way that leads to development of long-term dependence on the substances and in extreme situations to overdose related deaths. While cases of overdoses require emergency medical attention, long-term rehabilitation of addicted patients benefits from psychiatric care. Addiction relief can be achieved using a combination of medications and motivation enhancement psychotherapy (to keep patients focused on their goal of quitting) in a closely monitored medical setting.
Common mental disorders reported at specific life stages
While psychiatric illnesses might affect people at any age, treatment is often sought for specifically addressing behavioural problems in children or in the elderly.
Common childhood psychiatric disorders that child psychiatrists are frequently presented with are Attention Deficit Hyperactive Disorder (ADHD) where the affected patient is inattentive, restless, and impulsive.
ADHD can be managed using medicines and behavioural therapies focused on teaching patients and their families are effective ways to communicate. Children with autism (a condition marked by difficulty in perceiving social cues and in communicating, and stereotype repetitive behaviour) and mental developmental disorders (formerly referred to as ‘mental retardation’) are also frequently presented at psychiatric clinics. Behavioural therapies designed to help patients better communicate their needs to their family are the most common ‘treatments’ used. Though no cure is available for these conditions, intervening at an early age and teaching affected children to manage their situations despite their disabilities, leads to better outcomes overall, and is highly recommended.
Disorders seen frequently in elderly patients are of various types. Dementia such as Alzheimer’s disease and dementia following strokes. While there is so far no cure for these conditions, other problems such as anxiety and depression that often accompanies dementia needs to be managed by trained professionals to promote the patient’s well-being.













